What is health provider application to appeal a claims' determination?
A contracted provider dispute is a provider's written notice challenging, appealing or requesting reconsideration of a claim that has been denied, adjusted or contested or seeking resolution of a billing determination or other contract dispute or disputing a request for reimbursement of an overpayment of a claim. Health Care Provider Application to Appeal a Claims Determination is filled and submitted with determination in cases that resulted in the claim not being paid at all for reasons other than a UM determination or a determination of ineligibility, coordination of benefits or fraud investigation; Resulted in the claim being paid at a rate you did not expect based upon the contract of the health benefit plan.
Is health provider application to appeal a claims' determination Accompanied by Other Documents?
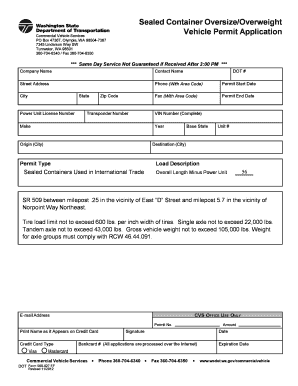
Each contracted provider dispute must contain, at a minimum, the following information: provider's name, billing provider's tax ID number, provider's contact information, and original claim form number, a clear identification of the disputed item, the Date of Service and a clear explanation of the basis upon which the provider believes the payment amount, request for additional information, request for reimbursement for the overpayment of a claim, contest, denial, adjustment or other action is incorrect.
What Information do I Provide in health provider application to appeal a claims' determination?
A separate application must be complete for each claim. Signatures must be legible, each form must be dated. Every application should contain: Provider Name, TIN/NPI, Provider Group (if applicable), Contact Name, Address, Phone, Fax, E mail. The claim should contain Patient's Name and ID. There are several questions that do not require written answers, the applicant should tick the appropriate box instead. Questions like ? Thea'SAS segment of benefits?” The Consent to Representation in Appeals of Utilization Management Determinations and Authorization to Release of Medical Records for UM Appeal and Arbitration of Claims?” Consent form is required for review of medical records if the matter goes to arbitration: Claim Number, Date of Service, Authorization Number, Claim filing method, Dispute of a denied claim ?provide date of denial, Additional information.
When and Where do I Send health provider application to appeal a claims' determination?
Contracted provider disputes must be received within 365 calendar days from the original action that led to the dispute or the most recent action if there are multiple actions that led to the dispute, or in the case of inaction, contracted provider disputes must be received within 365 calendar days after denying a claim or most recent claim has expired.